Infectious Spondylitis – An Operationally Relevant Disease?
From the Department of Anaesthesiology, Intensive Care Medicine, Emergency Medicine and Rescue Service1 (Chief Physician: Captain (MC) M. Benker, MBA) and the Department of Traumatology and Orthopaedics2 (Chief Physician: Colonel (MC) Prof. C. Willy) of the Bundeswehr Hospital Berlin (Hospital Commander: Captain (MC) Dr K. Reuter)
Stefan Markoff1, Clemens Richter1, Juliane Ruft2
Summary
Background: Untreated infectious spondylitis is a life-threatening disease, which often originates from a pyoderma. Pyodermas, in particular those acquired in tropical regions, often have complicated clinical courses resulting from infections with Staphylococcus aureus with and without a resistance to methicillin, but also with particular pathogenicity factors. Military personnel in tropical theatres of operations are exposed to an increased risk of infection by such pathogens.
Case description: We present a case of a 37 years old soldier who suffered from a trivial trauma of his right knee leading to a pyodermia and consecutively to a infectious spondylitis of his 11. thoracic spine. After repatriation to the Bundeswehr military hospital in Berlin intensive care including ventilation and conservativ ortopedic therapy had to be applied.
Discussion: This case shows that isolated local back pain without neurological symptoms, combinded with elvated markers of inflammation, can point out to a spondylitis/spondylodiszitis which immediately needs further diagnostics and antibiotic therapy. In patients suffering from pyodermial – time related to a stay in tropical areas – an infection with panton-velentine-leukzidin (PVL) producing staphylococci has to be taken into account. Staying in communal accodomation – as usual for military missions – facilitates spreading of those bacteria. An appropriate hygiene regimen for the purpose of prevention and during treatment of patients is of high importance.
Conclusions: Soldiers deployed to tropical regions are at risk to aquire a pyodermia induced by PVL-building -staphylococci. This increases the risk to develop infectious spondylitis. Isolated back pain without neurological symptoms must alert the treating physician to perform necessary diagnostical and therapeutical procedures including x-ray examination and profound microbiological lab tests. If a spondylitis is suspected initially a calculated and later resistance adapted antibiotic therapy is the pillar of each treatment. An antibiotic therapy of pyodermia acquired in tropical regions should be discussed. In case of a pyodermia a microbiological examination has to be targeted.
Keywords: spondylitis/spondylodiscitis, pyodermia, PVL-Sta-phylo-coccus aureus, antibiotics
Introduction

Back pain is one of the most frequent reasons for seeing a doctor, even in the regional medical treatment facilities of the Bundeswehr. Back pain can be a symptom of a multitude of diseases and conditions, of which acute trauma, degenerative diseases, slipped discs and excessive strain from unaccustomed activity are just a few examples.
Infectious spondylitis is a clinical condition that requires particular attention. Often it is only diagnosed after the disease has been present for a considerable amount of time and successful treatment of the disease is complex. The significant role pyodermas play in the development of infectious spondylitis shows the military medical importance of this condition, in particular in view of the extended task spectrum and the current and future theatres of operation of the Bundeswehr, as pyodermas are often found in patients returning from tropical regions.
Case report
A 37-year-old patient was repatriated from the EUTM[1] mission in Mali. He was evacuated from Mali via STRATAIRMEDEVAC and admitted to the interdisciplinary intensive care unit of the Bundeswehr Hospital in Berlin[2] .
Patient history
During his deployment, the patient complained of progressive back pain after physical exercise. Initially, it was assumed that he was suffering from a joint dysfunction of the thoracic spine or a problem involving the intervertebral discs. When he reported febrile temperatures and very severe back pain, he was assumed to be suffering from meningitis, and antibiotic treatment with ampicillin/sulbactam and ceftriaxone was started, as well as antiviral treatment with aciclovir. With further increasing inflammatory parameters and a left shift in the differential blood count, the aciclovir treatment was stopped, treatment with ciprofloxacin was started and the repatriation of the service member to Berlin via the PECC[3] in Koblenz was initiated.
Prior to suffering back pain, the service member had fallen and sustained a graze on the right knee, which was initially given little attention. Three weeks after this minor trauma, the service member came to see the unit physician. There had been a discharge of pus from the wound and the wound had been flushed with an antiseptic solution. Shortly after that, an abscess of approximately 2 x 2 cm developed on the right thigh; it was lanced and flushed under local anaesthesia (Figure 1). No swab was taken at that time.
Clinical findings
On admission to the Bundeswehr Hospital in Berlin, the patient was found to experience pain on percussion and vibration of the thoracolumbar junction. He scored 5/5 on both sides in Janda's muscle function test. He also had average reflexes on both sides. There were no neurological symptoms, the Lasègue test was negative on both sides and there was no meningism. Respiration was tachypnoeic with use of accessory muscles of respiration. The patient had increased respiratory sounds on both sides. In order to ensure sufficient oxygenation, the patient received continuous oxygen insufflation at 8 l/min. The patient had scleral icterus.
Diagnosis
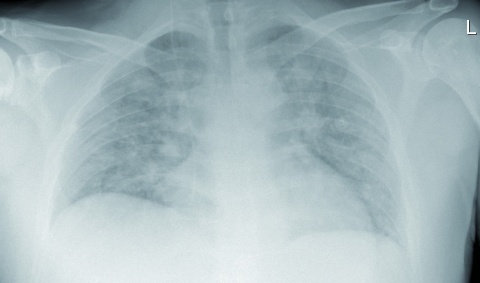
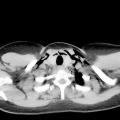
The X-ray image of the thorax showed pulmonary infiltrates on both sides without evidence of caverns (Figure 2). CT[4] scans of the thorax and abdomen with a contrast medium showed evidence of diffuse pulmonary infiltrates and pleural effusion on both sides as well as hepatosplenomegaly. MRI[5] scans of the thoracic and lumbar spine (native and with a contrast medium) revealed an isolated spondylitis of the 11th thoracic vertebra with circular paravertebral inflammatory response without involvement of the spine or the disc (Figure 3). Cardiac valvular vegetations were excluded by transoesophageal echocardiography. Viscous putrid secretions were obtained by bronchoscopy and microbially examined. Infection with malaria, tuberculosis, brucellosis, leptospirosis, hepatitis, HIV and legionella was ruled out. Apart from hepatosplenomegaly, the sonography of the abdomen was unremarkable. Laboratory tests on admission to the hospital detected increased inflammatory parameters, a left shift in the differential blood count and cholestasis. Staphylococcus aureus and Panton–Valentine leukocidin were detected in the blood cultures. No pathogens could be identified in the material obtained by bronchoscopy, but haematogenous dissemination and subsequent pneumonia are not unlikely.
Treatment and course of the disease
Initially, the patient required ventilation. A non-invasive method was used for ventilation (Figure 4).
According to the recommendations of Abele-Horn et al., antibiotic therapy was changed to empiric treatment with clindamycin, flucloxacillin, ceftriaxone [1] and – because initially a gram-negative infection of the respiratory tract could not be ruled out – also ciprofloxacin. The working group of Fleege et al. also recommends combining a third-generation cephalosporin antibiotic (cefotaxime) with flucloxacillin for initial empiric therapy [8]. After conclusive microbial diagnosis, antibiosis was adapted by switching to flucloxacillin and fosfomycin. Treatment with clindamycin was discontinued when resistance to this antibiotic was established. The patient received intravenous therapy for a total of 14 days and then received rifampicin and levofloxacin orally for a further four weeks.
The antibiotic treatment was adjusted in an interdisciplinary approach with the involvement of Laboratory Department I (microbiology) at the Berlin branch of the Central Institute of the Bundeswehr Medical Service Kiel within the framework of antibiotic stewardship established at the Bundeswehr Hospital in Berlin.
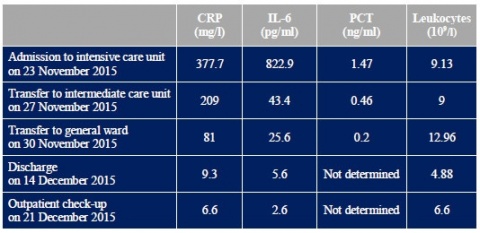
During treatment, the patient's inflammatory parameters regressed completely (see Table 1) and his gas exchange normalised. In consultation with the department for hospital hygiene, the patient was put into isolation owing to the detection of Staphylococcus aureus with PVL. After spending eight days in the intensive care and intermediate care units, he was transferred to the general ward. While he was still in the intensive care unit, the patient was fitted with a 3-point hyperextension brace so he could be mobilised to stand and walk while preventing axial rotation of the spine (Figure 5). On the general ward, mobilisation could be continued and extended as tolerated and under radiological control. Wearing the brace, the patient was able to stand for longer and walk increasing distances.
.
Discussion
General information on the disease
The clinical picture of infectious spondylitis was known even in ancient times [9], but the disease was first described by Lannelongue in 1879. Kolowski published a detailed account of spondylitis in 1936. He already suspected its cause to be haematogenous dissemination of bacteria [14].
The terms "spondylitis" and "spondylodiscitis" are mostly used interchangeably. Spondylitis is osteomyelitis of the spine, an infection of the vertebral bodies, which causes a secondary infection of the intervertebral discs. Spondylodiscitis is a primary infection of the intervertebral discs, which causes a secondary infection of the vertebral bodies [4, 6, 7, 9, 15].
Both entities are extremely complex and are frequently diagnosed at a very late stage, since there is a multitude of possible pathogens, incidence rates are low and clinical courses are very heterogeneous [10]. Owing to an often protracted period between the appearance of the first symptoms and a definitive diagnosis, it is very difficult to distinguish the two entities. In both cases, the disease is predominantly caused by a bacterial mono-infection, which can be most effectively treated by targeted antibiosis [12].
Depending on the literature, incidence of the disease ranges from 1:100 000 to 1:250 000 [5, 14]. Men are affected much more frequently. Risk factors include diabetes mellitus, malnutrition, tumours, HIV infections, taking steroids and rheumatic disorders.
The mortality rate was still 40–90% in the first half of the 20th century but could be reduced to approximately 5% today due to better diagnostics, more comprehensive knowledge and a wider spectrum of antibiotic treatment options [14]. Due to the increasing use of immunomodulatory substances and immunosuppressive therapies and the growing number of cases of tuberculosis even in Germany [17], however, an increase in cases of infectious spondylitis must be expected [12].
Microbiology
Generally, a wide array of bacteria, fungi and parasites can cause such an infection. Unspecific spondylitis is most commonly caused by staphylococci (39%), with Staphylococcus aureus heading the list with 36% of cases. The second and third most common causative agents are gram-negative bacteria and streptococci [18].
In the past few years, there have been reports of a change in the spectrum of pathogens. This was caused by an increase in tuberculosis cases [17] after years of decrease and by the increasing occurrence of gram-negative bacteria in drug addicts [14]. In tuberculosis patients who are not infected with HIV, tuberculosis affects the bones in up to 5% of cases, compared to up to 60% in those who are HIV positive. Fifty percent of all cases of osseous tuberculosis involve the spine [18].
The course of the infection is largely influenced by the virulence factors specific to the pathogens. PVL is an important factor that is produced both by community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) and by methicillin-sensitive Staphylococcus aureus (MSSA) [3]. Leukocidins cause lysis of leukocytes and tissue necrosis. In particular, necrotising pneumonia is a feared complication of an infection with PVL-producing staphylococci [13].
Routes of infection
A distinction is made between the endogenous and the exogenous routes of infection in spondylitis. The endogenous route is characterised by an infection unconnected with the vertebrae and subsequent haematogenous dissemination of pathogens [18]. The infection has a wide range of possible sources. These include the skin, soft tissue, the respiratory and urinary system. In most cases, the original source of infection can no longer be detected [2, 16, 20]. The exogenous route of infection is considerably less common. The causes of infection in these cases are usually surgical procedures or injections close to the spine [18].
Risk factors
Staphylococcus aureus with modified virulence properties is common in tropical regions. Pyodermas among travellers often have a complicated clinical course, with the travellers contributing to the spread of virulent staphylococci in temperate climatic zones after their return. During the treatment of patients who suffer from pyodermas after returning from tropical regions, medical staff must expect to deal with particularly virulent and multi-resistant pathogens [23].
Another risk factor for the transmission of these pathogens is communal accommodation. Higher transmission rates, however, can also be observed among athletes who share equipment and engage in contact sports. The pathogens can also be transmitted by vectors such as towels and other personal effects.
Clinical presentation
Patients with infectious spondylitis exhibit a wide and above all unspecific range of symptoms. The main symptom is localised back pain, which occurs in 85% of cases. Approximately half of the patients have a fever, a third suffer from neurological symptoms. Overall, it must be said that diagnosis is often delayed due to the broad differential diagnosis of back pain[11].
Diagnosis
In cases of suspected spondylitis, a combination of imaging (preferably magnetic resonance imaging), laboratory findings (above all inflammatory parameters) and microbiological diagnosis for pathogen identification is the most expedient approach. Blood cultures reveal important information for microbiological diagnosis. Taking blood cultures is the easiest, most economic and effective method of pathogen identification [12]. In order to increase the probability of successful pathogen identification, at least three pairs of blood cultures should be obtained before starting the antibiotic treatment. CT-guided biopsies may also be carried out to obtain test material [10]. Pathogen identification, however, which is a prerequisite for targeted antibiotic treatment, only succeeds in 35 to 83% of cases of infection [12].
Treatment
Treatment of infectious spondylitis should be planned by an interdisciplinary team consisting at least of microbiologists, internists, spinal surgeons and, in the event of serious complications, intensive care physicians. As a rule, it is important to consider two treatment options – conservative treatment with strict immobilisation on the one hand and surgical treatment on the other. The surgical treatment option should be considered in cases of severe sepsis and advanced osseous destruction.
The cornerstone of both treatment options is antibiotic therapy. When clinical findings lead to a suspicion of infectious spondylitis, empiric antibiotic treatment must be initiated immediately. This empiric treatment of an (as yet) unknown pathogen includes a combination therapy consisting of, for example, flucloxacillin, ceftriaxone and clindamycin [1]. It exploits the effectiveness of isoxazolyl penicillins against Staphylococcus aureus as a frequent cause of spondylitis. However, isoxazolyl penicillins are unreliable when dealing with streptococci and ineffective against gram-negative pathogens. This is compensated by combination with a third-generation cephalosporin. Clindamycin inhibits bacterial protein synthesis and thus the production of toxins by group A streptococci and possibly also by Staphylococcus aureus. This makes it an important combination partner for the treatment of infections in which the toxin effect is the main focus. Its effect ranges from bacteriostatic to bactericidal and depends on its concentration and the pathogens involved [19]. Clindamycin also has excellent bone penetration [8]. As in our case, however, clindamycin resistance is common.
Antibiotic treatment should be conducted for at least six weeks in uncomplicated cases and for up to three months in complicated cases [10].
Conclusions and military medical aspects
In the case described above, development of spondylitis via an endogenous route of infection is likely. The infection could have originated from a minor injury of the knee or an abscess of the thigh, between which there may also have been a connection. As no bacteriological analysis was performed in either case, there is no definite evidence for the exact route of infection. An exogenous infection, however, is unlikely due to the patient's history (no spinal injections or spinal surgery).
Antibiosis for pyodermas?
Of military medical importance is the question of whether therapy of skin abscesses, in particular in tropical theatres of operation, should include (perioperative) antibiotic prophylaxis or an antibiotic treatment in addition to local treatment in order to avoid any further complications such as infectious spondylitis.
There are currently no special recommendations for patients returning from tropical regions with pyodermas[21]. On the basis of available data, it is thus impossible to make general recommendations concerning antibiotic prophylaxis for abscess lancing. Systemic antibiotic treatment may, however, become necessary at the latest if military personnel in theatres of operation, as well as those with similar symptoms at home, suffer recurring skin infections [23].
In the case of abscesses, it is essential to take swabs for further microbiological diagnosis before starting antibiotic treatment. When planning the medical aspects of operations abroad, appropriate documented procedures must be established for the shipping and processing of microbiological test material and for the timely transmission of findings. The development of test methods that do not require a complete bacteriological laboratory, and the enhancement of telemicrobiology capabilities, could also be taken into consideration.
A bacteriological examination (swab) should always be performed on patients with pyodermas who visit the unit physician after returning from tropical countries.
Immediate action is required
Isolated back pain without neurological symptoms, in combination with highly elevated inflammatory parameters, may indicate spondylitis/spondylodiscitis and requires immediate diagnostic clarification and antibiotic treatment. A combination therapy with clindamycin, flucloxacillin and ceftriaxone is currently recommended for the initial empiric antibiotic treatment of this disease [1].
Preventive measures
As part of the in-processing in theatres of operation, the unit physicians and/or health supervisors of operational forces should brief personnel on the increased risk of transmitting virulent pathogens in communal accommodation and by sharing articles of daily use. As transmission occurs through direct skin/hand contact with infected patients and through direct contact with objects they have contaminated or clothes they have worn (and which have not been washed), there is no fully effective protection against an infection with PVL-producing staphylococci. The risk of infection may be reduced by frequently washing and disinfecting the hands. Wounds and scratches should be covered with adhesive plasters; sharing towels and other personal effects must be avoided.
Hygiene measures
If military personnel are repatriated on suspicion of these diseases or because of confirmed systemic complications, an appropriate prophylactic hygiene regime must be observed both during transport and in the admitting hospitals.
Those interacting with and caring for affected patients must wear face masks, disposable gowns and gloves and thoroughly disinfect their hands before entering the patient's room and after taking off the gloves. If PVL-producing staphylococci are detected in patients or their relatives/contact persons, we recommend carrying out what is known as decolonisation treatment involving the application of nasal ointment, antiseptic lavages and mouth rinses [22].
Conclusions
Infectious spondylitis is an operationally relevant disease. The unit physician in theatre should be familiar with its symptoms, diagnosis and therapy as well as prevention and hygiene measures.
Key statements
- Isolated back pain with elevated inflammatory parameters may be a symptom of spondylitis.
- In addition to a thorough clinical examination, diagnosis includes conclusive imaging and microbiological examinations.
- Antibiotic therapy is the focus of treatment of infectious spondylitis.
- Pyodermas in tropical theatres of operation are a significant endogenous route of infection. In such cases, medical staff must expect to deal with particularly virulent and multi-resistant pathogens.
- A microbiological examination should be the standard procedure even when treating infected minor injuries and/or lancing skin abscesses.
References
- Abele-Horn M, Heinz W: Antimikrobielle Therapie. Entscheidungshilfen zur Behandlung und Prophylaxe von Infektionskrankheiten, 3. Auflage. Marburg: Wiehl 2010.
- Akbar M, Lehner B, Doustdar S, et al.: Pyogene Spondylodiszitis der Brust- und Lendenwirbelsäule. Eine neue Klassifikation zur Entscheidungsfindung bei der Wahl der operativen Therapie. Orthopäde 2011; 40(7): 614-623.
- Becker K, Kriegeskorte A, Sunderkötter C, Löffler B, von Eiff C: Chronisch rezidivierende Infektionen der Haut und Weichgewebe durch Staphylococcus aureus. Klinische Bedeutung des Small-colony-variant (SCV)-Phänotyps und von Panton-Valentine-Leukozidin (PVL)-positiven S.-aureus-Isolaten. Hautarzt 2014; 65(1): 15-25.
- Klöckner C, Valencia R, Weber U: Die Einstellung des sagittalen Profils nach operativer Therapie der unspezifischen destruierenden Spondylodiszitis: ventrales oder ventrodorsales Vorgehen -ein Ergebnisvergleich. Orthopäde 2001; 30: 965-967.
- Chelsom J, Solberg CO: Vertebral osteomyelitis at a Norwegian university hospital 1987-97: clinical features, laboratory findings and outcome. Scand J Infect Dis 1998; 30(2): 147-151.
- Cramer J, Haase N, Behre I, Ostermann PAW: Spondylitis und Spondylodiszitis. Trauma und Berufskrankheit 2003; 5(3): 336-341.
- Eysel P, Hopf C, Meurer A (1994) Korrektur und Stabilisierung der infektbedingten Wirbelsäulendeformität. Orthopädische Praxis 1994;(11): 696-703.
- Fleege C, Wichelhaus TA, Rauschmann M: Systemische und lokale Antibiotikatherapie bei konservativ und operativ behandelten Spondylodiszitiden. Orthopäde 41(9): 727-735.
- Frangen TM, Kälicke T, Gottwald M, Andereya S, et al.: Die operative Therapie der Spondylodiszitis. Eine Analyse von 78 Patienten. Unfallchirurg 2006; 109(9): 743-753.
- Huttner B, Opravil M: Die infektiöse Spondylitis. Z Rheumatol 2006; 65(1): 7-11.
- Jung N, Seifert H, Siewe J, Fätkenheuer G: Spondylodiszitis. Internist (Berl) 2013; 54(8): 945-953.
- Lehner B, Akbar M, Rehnitz C, et al.: (2012) Standards der mikrobiologische Diagnostik der Spondylodiszitis. Orthopäde 2012; 41(9): 702-710.
- Lina G, Piémont Y, Godail-Gamot F, Bes M, et al.: Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis 1999; 29(5): 1128-1132.
- Mickley T, Kirschner M, Hierholzer C, Hofmann GO: Spondylitis-Spondylodiszitis. Trauma und Berufskrankheit 2003; 5(0): 296-304.
- Peters KM, Klosterhalfen B, Eysel P: Bakterielle Infektionen der Knochen und Gelenke. Bücherei des Orthopäden, Bd 69. Stuttgart: Enke 1997.
- Renker EK, Möhring K, Abel R, et al.: Urogene Spondylodiszitis. Orthopäde 2009; 38(4): 355-364.
- Robert Koch-Institut: Tuberkulose in Deutschland: Ende des rückläufigen Trends? RKI-Bib1. Berlin: Robert-Koch-Institut 2015.
- Sobottke R, Seifert H, Fätkenheuer G, Schmidt M, Goßmann A, Eysel P: Aktuelle Diagnostik und Therapie der Spondylodlszitis. Dtsch Ärztebl 2008; 105(10): 181 -187.
- Sunderkötter C, Becker K: Systemtherapie mit Antiinfektiva. Hautarzt 2014; 65(2): 113-124.
- Vos FJ, Kullberg BJ, Sturm PD, Krabbe PFM, et al.: Metastatic infectious disease and clinical outcome in Staphylococcus aureus and Streptococcus species bacteremia. Medicine (Baltimore) 2012; 91(2): 86-94.
- Wacha et al.: Perioperative Antibiotikaprophylaxe. Empfehlungen einer Expertenkommission der Paul-Ehrlich-Gesellschaft für Chemotherapie e.V. Chemother J 2010; 19(3): 70-84.
- Witte W, Wiese-Posselt M, Jappe U: Community MRSA. Hautarzt 2005; 56(8): 731-738.
- Zanger P: Staphylogene Pyodermie bei Tropenrückkehrern-Reisende importieren virulente und resistente Stämme. Flug u Reisemed 2013; 19(06): 272-275.
Photos:
Alle Abbildungen Bundeswehrkrankenhaus Berlin; Einverständnis des Patienten zur Veröffentlichung wurde erteilt.
Conflicts of interests:
Die Autoren, die zu gleichen Teilen an dieser Arbeit mitgewirkt haben, erklären, dass keine Interessenkonflikte bestehen.
Manusckript data:
Eingereicht: 18.12.2015
Revidierte Fassung angenommen: 08.04.2016
Citation:
German:
Markoff S, Richter C, Ruft J: Die infektiöse Spondylitis – eine einsatzrelevante Erkrankung? Wehrmedizinische Monatsschrift 2016; 60(45): 136-141.
English:
Markoff S, Richter C, Ruft J: Infectious spondylitis – a military operations related disease? Wehrmedizinische Monatsschrift 2016; 60(5): 136-141.
Corresponding author:
Oberfeldarzt Dr. Stefan Markoff
Bundeswehrkrankenhaus Berlin
Abteilung X Anästhesie, Intensivmedizin, Notfallmedizin
und Rettungsdienst
Scharnhorststr. 13, 10115 Berlin
E-Mail: [email protected]
Eine deutsche Version des Textes finden Sie hier.
A german version of this article you will find here.
- [1] European Training Mission
- [2] Strategic Aeromedical Evacuation
- [3] Patient Evacuation Coordination Centre
- [4] Computed tomography
- [5] Magnetic resonance imaging
Datum: 14.07.2016
Quelle: Wehrmedizinische Monatsschrift 2016/5