Heat acclimation for attenuation of heat risk and performance -enhancement in military operations
From the United States Air Force Exercise Science Unit (Chief: Dr. N. Baumgartner) of the United States Air Force Personnel Center, Joint Base San Antonio-Randolph, Texas (Commander: Major General B. T. Kelly)
Summary
Background: Protective clothing and gear restrict heat dissipation during military operations in both hot and cool environments placing military personnel at an elevated risk for heat injury/illness. Fairly complex and expensive technologies are employed to address this problem, however, heat acclimation (HA), an intervention occasionally used in athletics, is not often considered in military operations and training.
Discussion: Well known HA-induced physiological adaptations are, temporally, cardiovascular changes followed by enhanced sweat mechanisms resulting in reduced thermoregulatory strain. However, HA may be of little or no use in military operations as these adaptations, namely enhanced sweat mechanisms, are restricted by required military clothing and gear. The US Air Force conducted thermal stress research to explore if HA was efficacious for addressing thermal strain in military operations. We measured thermal stress in subjects exercising in warm-humid conditions while wearing the bulky, heat transfer restricting US Air Force Chemical Defense Ensemble (CDE) prior to and after ten days of hot-humid HA. Heat balance equations showed that HA elicited significantly lower thermal stress during exercise in the CDE, this result was not due to enhanced heat dissipation mechanisms, rather due to reduced metabolic heat production. Finally, we provide applied physiology recommendations to elicit a state of HA in military personnel prior to conducting operations in varied climate conditions.
Conclusion: Due to its effect on exercise metabolic rate HA may offer a low cost methodology for attenuating heat injury risk and concomitantly enhancing human performance in military members wearing semi-permeable or non-permeable clothing in both cool and hot environments
Keywords: heat acclimation, heat acclimatization, exercise, human performance, military operations
Zusammenfassung
Hintergrund: Schutzbekleidung und -ausrüstung behindern die Wärmabgabe und erhöhen bei Einsätzen sowohl in heißer wie in kalter Umgebung das Risiko für hitzestressinduzierte Erkrankungen. Zur Lösung dieses Problems wurden komplexe und kostenaufwändige Technologien entwickelt. Die Möglichkeit des Trainings zur Hitzeanpassung (Heat Acclimation, HA), wie es gelegentlich im Sport angewandt wird, wurde bisher aber kaum in die Überlegungen zur Einsatzvorbereitung einbezogen.
Diskussion: Die bekannten Effekte der HA zur Verringerung der Hitzewirkung betreffen zunächst das Herzkreislaufsystem, gefolgt von einer Steigerung der Schweißsekretion. Insbesondere der Beitrag der verbesserten Schweißsekretion ist dabei im militärischen Kontext durch Bekleidung und Ausrüstung limitiert.
Die US Air Force hat untersucht, ob HA -Training die Fähigkeiten von Soldaten zum Umgang mit Hitzebelastungen bei militärischen Operationen verbessert. Dazu wurde der Hitzestress bei Personen, die in feucht-warmer Umgebung die sperrige, wärmeisolierende US Air Force ABC-Schutzausrüstung (CDE) trugen, vor und nach einem 10-tägigen HA-Training in feucht-heißer Umgebung erfasst. Vergleiche der Wärmebilanzen zeigten, dass HA-Training zu einem signifikant niedrigeren Hitzestress bei Übungen unter CDE führten. Dieses Ergebnis ist nicht auf eine verbesserte Wärmeabgabe, sondern vielmehr auf eine geringere metabolische Wärmeproduktion zurückzuführen. Für die US Air Force wurden deshalb Empfehlungen aus Sicht der angewandten Physiologie herausgegeben, um einen angemessenen HA-Trainingsstatus bei militärischen Personal vor Entsendung in heiße Klimazonen zu erreichen.
Schlussfolgerungen: HA-Training mit seinem positiven Einfluss auf den Energieumsatz unter Hitzebelastung eröffnet kostengünstige Möglichkeiten, sowohl das Risiko für das Auftreten hitzeinduzierter Erkrankungen zu reduzieren als auch die Leistungsfähigkeit des Personals – insbesondere beim Tragen von semi-permeabler oder nicht permeabler Bekleidung, wie z. B. ABC-Schutzausrüstung – unter allen klimatischen Bedingungen zu verbessern.
Schlüsselwörter: Hitzeanpassung, Hitzeakklimatisation, kör-perliche Arbeit, menschliche Leistungsfähigkeit, militärische Einsätze
Introduction
During exercise in a hot environment one will experience greater physiological strain than that experienced during exercise of the same intensity and duration performed in a thermo-neutral or cool environment. The heat load stimulates higher levels of sweating and cutaneous blood flow resulting in increased difficulty in maintaining fluid-electrolyte balance and cardiovascular stability. However, the body has the ability to adapt or acclimate to the combined stress of internal heat generation and external heat load. Thermal physiologists define heat acclimation (HA) as the adaptive changes that occur when one undergoes repeated or prolonged heat exposure and the concomitant reduction in physiological strain produced by a hot environment. HA is produced by repeated exposure to a heat stress sufficient to raise internal body temperature to levels that provoke moderate to profuse sweating, and is most effectively accomplished by exercise in the heat [29, 32]. The terms heat acclimation and heat acclimatization are frequently used interchangeably; however, the recommendation of the International Union of Physiological Sciences states:
Heat acclimation |
Heat acclimatization |
Heat acclimation – Salient characteristics
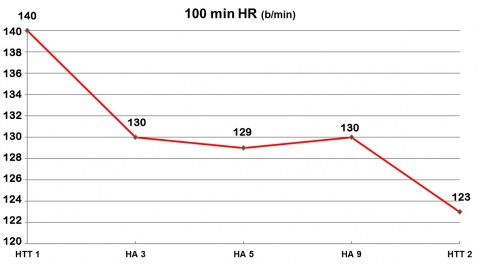
- Decreased exercise heart rate, 2 - 6 days [3, 14, 20, 21, 24, 26, 27]
- Increased resting plasma volume, 2 - 6 days [3, 16, 24]
- Improved defense of plasma volume during exercise-heat stress [3, 24]
- Increased resting and exercise stroke volume, 2 - 6 days [3, 16, 24]
- Increased heat loss via radiation and convection, 3 - 10 days [3, 19]
- Decreased rating of perceived exertion, 3 - 6 days
- Decreased resting core temperature, 5 - 12 days [3, 16]
- Decreased exercise core temperature, 5 - 12 days [3, 14, 16, 20, 21, 26, 27]
- Decreased exercise skin temperatures, 5 - 12 days [3, 16]
- Decreased sodium chloride losses in sweat and urine, 5 - 10 days [1, 3, 8]
- Increased sweat rate, 7 - 14 days [3, 16, 31]
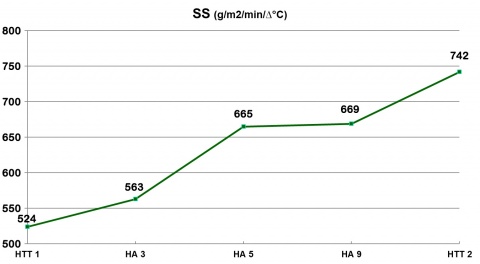
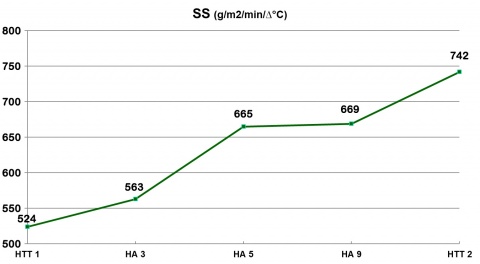
- Increased sweat sensitivity, i.e., greater sweat production per change in rectal temperature (Tc) [3, 9, 31]
- Increased exercise tolerance time
- Decreased exercise metabolism [2, 3, 22]
These adaptations are for healthy well-nourished, adequately hydrated subjects. The result of the above physiological adaptations is an improved transfer of heat from the body’s core to the skin and from the skin to the environment [3, 29].
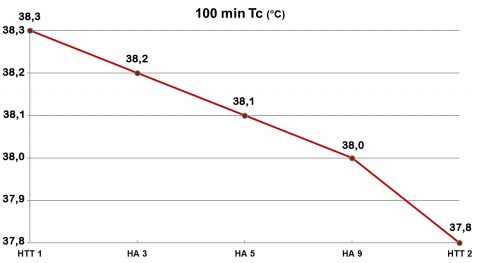
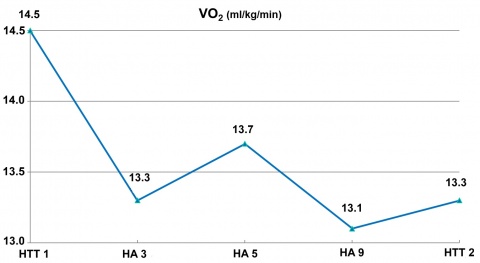
HA data from a US Air Force (USAF) thermal stress research protocol [6, 30] demonstrate the above. Eight males (age 27.2 ± 4.8 yrs, mass 72.3 ± 8.4 kg, maximum oxygen uptake (VO2 max) 55.1 ± 6.6 ml O2 kg-1 min-1) completed heat tolerance tests (HTT 1 and HTT 2) before and after nine consecutive days of HA. Both the HTT and HA trials consisted of 100 minutes walks at 25 % VO2 max in hot-humid conditions 43.1 ± 0.1 °C DB (dry bulb), 50.0 ± 0.1 % relative humidity (RH), 33 mmHg vapor pressure (VP). We measured rectal temperature (Tc), heart rate (HR), VO2, and sweat sensitivity (SS) during the HTTs and HA trials 3, 5 and 9. Subjects achieved HA as indicated by HTT 1 vs HTT 2 (see figures 1, 2 and 3).
Heat acclimation- Useful in military training and operations?
If heat dissipation is attenuated or completely shut off, is there any value in HA? Some claim that HA is not useful in the military setting. YAMAZAKI [35] states, “HA improves endurance work performance in the heat and thermal comfort at a given work rate. In workers wearing personal protective suits in hot environments, however, little psychophysiological benefit is received from short-term exercise training and/or heat acclimation because of the ineffectiveness of sweating for heat dissipation and the aggravation of thermal discomfort with the accumulation of sweat within the suit.” However, HA affects both sides of the heat balance picture. The cardiovascular and thermoregulatory adaptations listed above increase heat dissipation, gains that are attenuated or eliminated in the military clothing/equipment microenvironment, but HA also elicits metabolic adaptations that attenuate heat generation, namely a reduction in exercise metabolic rate for a given work load, i.e., improved exercise economy (run and walk) or efficiency (cycling) [3, 11, 29]. This adaptation is quite viable for military training and operations as a reduction in exercise metabolic rate (lower oxygen uptake, a lower VO2 submax, at the same workrate) is a non-sweating means of affecting heat balance [18, 22, 36].
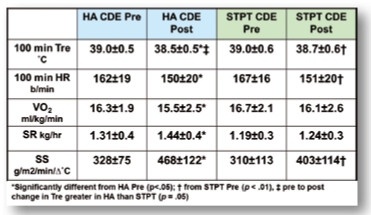
Our USAF data demonstrate the import of a HA-induced reduction in heat generation when one must don military gear that impairs heat dissipation, primarily evaporative heat loss. We studied the effects of heat acclimation and short-term physical training on exercise-heat tolerance in men wearing protective clothing. The USAF Chemical Defense Ensemble (CDE) consists of a two piece chemical protective overgarment, butyl rubber hood, mask, and gloves worn over standard military fatigues/air battle uniform [30]; clo value = 2.5 (see figure 6).The CDE impedes heat dissipation and its bulk (7.5 kg) decreases movement efficiency [25]. Numerous studies have documented the physiological strain imposed by CDE; higher Tc, Tsk, SS, HR, VO2, and sweat rate [4, 30, 7, 15, 28]. Mechanical modifications, e.g., water or air cooled vests, and modeling / prediction studies have been accomplished; however, can we alter physiological capability? We conducted exercise trials on 16 males (mean ± SD: age 26.3 ± 5.0 yrs, body mass 73.4 ± 7.6 kg, VO2 max 54.8 ± 6.2 mlO2 kg-1 min-1, body composition 14.3 ± 4.4 % fat, body surface area 1.90 ± 0.11 m2) wearing the CDE prior to and after 10 days of HA or 10 days of short term physical training (STPT), n = 8 each group [5].
Trial pattern:
CDE Test 1 (Pre) –> HA Treatment or STPT Treatment –> CDE Test 2 (Post)

In conclusion, HA increased exercise-heat tolerance in the CDE by increasing heat dissipation (limited amount in microenvironment), but primarily by reducing metabolic heat production. Although STPT had lesser effects than HA, it still provides an alternative procedure for improving work performance in the CDE.
Heat acclimation – Military application / applied physiology
Applied Physiology Recommendations
- Conduct moderate to long term (≥ 8 days) HA as possible, but at least conduct short term HA (≤ 7 days) prior to salient military training / operational events
- Dry vs Wet: match HA environment to military ensemble environment
- Prevent decay of HA via periodic (≈ two days/wk) exercise-heat exposures
- Maintain aerobic training in thermo-neutral or cool conditions
- Conduct HA in conjunction with routine physical training (PT), i.e., start HA immediately subsequent to PT as one will have already achieved an initial elevation in core temperature via PT
- Active HA (exercise in the heat) is superior to passive HA, e.g., insert cycle into sauna or thermal chamber
- Low cost set up: heater and humidifier in small room / wood box / attic / chamber (Figure 7)
- Recommend 100 % fluid replacement during HA trials to “train the gut”; increase efficiency in transferring fluid from small intestine to interstitial and intravascular spaces
- As possible, employ hyperthermic clamping, gradually increase environmental and metabolic stimuli to elicit same body temperature responses each HA trial day
- Assess core temperature via esophageal or rectal probes, temporary internal sensor “pills,” or employ heart rate-based models for predicting body temperature
- Beware of inter-individual variability; not all respond same
Recommendations / Policy Guidance
USAF Instruction 48 - 151, Thermal Injury Prevention Program, is available as a helpful reference for applied physiology use in military organizations. Finally, the application of science-based HA principles is an example of the key role military scientific organizations should perform by underpinning military training and operational policies and procedures with scientific basis and rationale. This will at times require solid leadership and communication to overcome the inertia inherent to military traditional-historical patterns that are not necessarily optimal. These patterns typically have been in place across military generations, but often lack a sound basis for application in training and operations.
The views expressed in this article are those of the author, and do not necessarily reflect official United States Government, Department of Defense, or Air Force positions or policies.
Literature
- Allan JR, Wilson CG: Influence of acclimatization on sweat sodium concentration. J Appl Physiol 1971; 30 (5): 708 - 712.
- Armstrong LE, Hubbard RW, DeLuca JP, Christensen EL: Heat acclimatization during summer running in the northeastern United States. Med Sci Sports Exerc 1987; 19 (2): 131 - 136.
- Armstrong LE, Maresh CM: The induction and decay of heat acclimatisation in trained athletes. Sports Med 1991; 12 (5): 302 - 312.
- Armstrong LE, Szlyk PC, Sils IV, Luca JP de, O’Brien C, Hubbard RW: Prediction of the exercise-heat tolerance of soldiers wearing protective overgarments. Aviat Space Environ Med 1991; 62 (7): 673 - 677.
- Baumgartner N, Byrne HK, Mier CM, Turley KR, Constable SH, Wilmore JH: Effects of heat acclimation and short-term physical training on exercise-heat tolerance in men wearing protective clothing. Aerospace Medicine and Human Performance (in preparation).
- Baumgartner N, Byrne HK, Mier CM, Turley KR, Constable SH, Wilmore JH: Individual effects of heat acclimation and short-term physical training on submaximal exercise metabolic rate. J Appl Physiol (in preparation).
- Bishop PA, Pieroni RE, Smith JF, Constable SH: Limitations to heavy work at 21 degrees C of personnel wearing the U.S. military chemical defense ensemble. Aviat Space Environ Med 1991; 62 (3): 216 - 220.
- Dill DB, Hall FG, van Beaumont W: Sweat chloride concentration: Sweat rate, metabolic rate, skin temperature, and age. J Appl Physiol 1966; 21 (1): 99 - 106.
- Frye AJ, Kamon E: Responses to dry heat of men and women with similar aerobic capacities. J Appl Physiol Respir Environ Exerc Physiol 1981; 50 (1): 65 - 70.
- Garden JW, Wilson ID, Rasch PJ: Acclimatization of healthy young adult males to a hot-wet environment. J Appl Physiol 1966; 21(2): 665 - 669.
- Houmard JA, Costill DL, Davis JA, Mitchell JB, Pascoe DD, Robergs RA: The influence of exercise intensity on heat acclimation in trained subjects. Med Sci Sports Exerc 1990; 22(5): 615 - 620.
- King DS, Costill DL, Fink WJ, Hargreaves M, Fielding RA: Muscle metabolism during exercise in the heat in unacclimatized and acclimatized humans. J Appl Physiol 1985; 59 (5): 1350 - 1354.
- Lorenzo S, Halliwill JR, Sawka MN, Minson CT: Heat acclimation improves exercise performance. J Appl Physiol 2010; 109 (4): 1140 - 1147.
- Maher JT, Bass DE, Heistad DD, Angelakos ET, Hartley LH: Effect of posture on heat acclimatization in man. J Appl Physiol 1972; 33 (1): 8 - 13.
- McLellan TM, Meunier P, Livingstone S: Influence of a new vapor protective clothing layer on physical work tolerance times at 40 degrees C. Aviat Space Environ Med 1992; 63 (2): 107 - 113.
- Mitchell D, Senay LC, Wyndham CH, van Rensburg AJ, Rogers GG, Strydom NB: Acclimatization in a hot, humid environment: Energy exchange, body temperature, and sweating. J Appl Physiol 1976; 40 (5): 768 - 778.
- Nadel ER, Pandolf KB, Roberts MF, Stolwijk JA: Mechanisms of thermal acclimation to exercise and heat. J Appl Physiol 1974; 37 (4): 515 - 520.
- Rivas E, Rao M, Castleberry T, Ben-Ezra V: The change in metabolic heat production is a primary mediator of heat acclimation in adults. J Therm Biol 2017; 70 (Pt B): 69 - 79.
- Roberts MF, Wenger CB, Stolwijk JA, Nadel ER: Skin blood flow and sweating changes following exercise training and heat acclimation. J Appl Physiol Respir Environ Exerc Physiol 1977; 43 (1): 133 - 137.
- Robinson S, Turrell ES, Belding HS, Horvath SM: Rapid acclimatization to work in hot climates. American Journal of Physiology-Legacy Content 1943; 140 (2): 168 - 176.
- Rowell LB, Kraning KK, Kennedy JW, Evans TO: Central circulatory responses to work in dry heat before and after acclimatization. J Appl Physiol 1967; 22 (3): 509 - 518.
- Sawka MN, Pandolf KB, Avellini BA, Shapiro Y: Does heat acclimation lower the rate of metabolism elicited by muscular exercise? Aviat Space Environ Med 1983; 54 (1): 27 - 31.
- Senay LC, Kok R: Effects of training and heat acclimatization on blood plasma contents of exercising men. J Appl Physiol Respir Environ Exerc Physiol 1977; 43 (4): 591 - 599.
- Senay LC, Mitchell D, Wyndham CH: Acclimatization in a hot, humid environment: Body fluid adjustments. J Appl Physiol 1976; 40 (5): 786 - 796.
- Speckman KL, Allan AE, Sawka MN, Young AJ, Muza SR, Pandolf KB: Perspectives in microclimate cooling involving protective clothing in hot environments. International Journal of Industrial Ergonomics 1988; 3 (2): 121 - 147.
- Strydom NB, Wyndham CH, Williams CG, et al.: Acclimatization to humid heat and the role of physical conditioning. J Appl Physiol 1966; 21 (2): 636 - 642.
- Taylor HL, Henschel AF, Keys A: Cardiovascular adjustments of man in rest and work during exposure to dry heat. American Journal of Physiology-Legacy Content 1943; 139 (4): 583 - 591.
- Thornton R, Caldwell JL: The physiological consequences of simulated helicopter flight in NBC protective equipment. Aviat Space Environ Med 1993; 64 (1): 69 - 73.
- Wenger CB: Human heat acclimatization. In: Sawka MN, Gonzalez RR, Pandolf KB (eds.): Human performance physiology and environmental medicine at terrestrial extremes. Dubuque, IA: Brown & Benchmark 1988; 153 - 197.
- Wilmore JH, Baumgartner N, Byrne HK, Mier CM, Radcliff JL: Effects of work rate and temperature on work/rest cycles when wearing the chemical defense ensemble (Final Report). USAF Armstrong Laboratory Technical Report 1997 - 0117.
- Wyndham CH: Effect of acclimatization on the sweat rate-rectal temperature relationship. J Appl Physiol 1967; 22 (1): 27 - 30.
- Wyndham CH: The physiology of exercise under heat stress. Annu Rev Physiol 1973; 35 : 193 - 220.
- Wyndham CH, Benade AJ, Williams CG, Strydom NB, Goldin A, Heyns AJ: Changes in central circulation and body fluid spaces during acclimatization to heat. J Appl Physiol 1968; 25 (5): 586 - 593.
- Wyndham CH, Rogers GG, Senay LC, Mitchell D: Acclimization in a hot, humid environment: Cardiovascular adjustments. J Appl Physiol 1976; 40 (5): 779 - 785.
- Yamazaki F: Effectiveness of exercise-heat acclimation for preventing heat illness in the workplace. J UOEH 2013; 35 (3): 183 - 192.
- Young AJ, Sawka MN, Levine L, Cadarette BS, Pandolf KB: Skeletal muscle metabolism during exercise is influenced by heat acclimation. J Appl Physiol 1985; 59 (6): 1929 - 1935.
Author
Dr. Neal Baumgartner
United States Air Force Exercise Science Unit
Joint Base Randolph, Texas 78150
United States of America
E-Mail: [email protected]
Datum: 27.10.2018