Deployment-Related Post-Traumatic Stress Disorder in Service Members from the Perspective of their Families and Relatives – Qualitative Evaluation of a Resource that can be Activated
Ulrich Wesemann, Swantje Radszat, Tabea Fischer, Carolyn Rose
Background: On average, more than 340 new cases of deployment-related mental disorders in personnel of the German armed forces are reported every year. The majority of affected service members do not, however, receive any professional help. How these psychological changes are perceived by families and relatives has not yet been investigated.
Methods: N = 47 family members and relatives of servicemen and women with deployment-related post-traumatic stress disorder were surveyed about their perception of the stress suffered by the service members concerned. The survey was conducted during workshops for family members that were held between 2011 and 2017. The qualitative evaluation was based on the six-phase process of thematic analysis developed by BRAUN and CLARKE.
Results: The family members and relatives identified the following problem areas pertaining to the servicemen and women in question: “feelings and emotions expressed”, “withdrawal and avoidance behaviour”, “aggression and hostility”, “communication”, “physical closeness”, “trust”, “physical symptoms”, “changes in personality and behaviour” and a “residual category”.
Discussion: The problems described could be easily categorised. All of the established categories directly or indirectly influence families and relatives. Although there is some overlap between these categories and the diagnostic criteria for PTSD according to the ICD-10, the problem areas of “physical closeness”, “communication” and “trust” could also be identified.
Conclusions: The families and relatives of affected servicemen and women often experience considerable strain. More specific measures to include families and relatives are recommended. The problem areas identified were intended as the basis for a questionnaire to be filled in by the families and relatives. If the information provided by respondents can be used to more rapidly diagnose and also classify the symptoms of affected servicemen and women, these service members are more likely to seek professional help at an earlier stage or even seek professional help at all. This could help to address one of the largest problems that currently exists in psychiatric care.
Keywords: Families and relatives of military personnel, post-traumatic stress disorder, hostility, quality of life, use of offers of help
Introduction
Deployments abroad have led to changes in the type and frequency of psychological symptoms among servicemen and women in the German armed forces (Bundeswehr) [2, 21, 24]. The significance of mental disorders caused by traumatic experiences and their effects on family members and relatives has increased considerably in medical care systems, not least because of international conflicts [18]. Mental disorders not only cause personal suffering but also have considerable economic consequences as a result of sick leave, reduced productivity, and unfitness for service. On average, more than 340 new cases of deployment-related mental conditions that are classified as a disorder have been reported annually among Bundeswehr personnel over the past six years and entered in the central database of operational statistics. The number of unreported cases is likely to be much higher [35]. Fear of stigma and illness-related avoidance behaviour are some of the reasons why patients rarely seek professional help [22]. Mental disorders are also widespread in the Bundeswehr.
The Bundeswehr Psychological Service, the Bundeswehr Social Services and the Bundeswehr Medical Service have undertaken various research efforts to address this issue. There are a number of Bundeswehr publications that discuss different disorders and symptom clusters such as sleep and nightmares [6, 8], tobacco and alcohol dependence [2, 23, 29, 37], depression and suicidal tendency [34, 36] and PTSD [4, 11, 15, 17], as well as papers on therapeutic strategies [13, 33, 37], prevention and efforts to prevent stigma [20, 26, 27] and on screening procedures [30]. Workshops, counselling services and extension training on this subject have also been implemented [1, 9, 14, 25]. The range of support services offered by the Bundeswehr is therefore varied and extensive. There is also a transfer of military expertise to the civil sector. As part of the terrorist attack in 2016 on the Breitscheidplatz in Berlin, the emergency responders were psychologically examined [28, 31].
However, Bundeswehr servicemen and women complained increasingly of interpersonal conflicts and their family members expressed the need to be more involved in treatment. They wished, among other things, for more information regarding their partner’s PTSD as well as advice and support to help them deal with persons suffering from PTSD [19]. Thus, the focus has recently shifted to the families. Owing to the support services that are now available for both military personnel and their families, interpersonal problems can be addressed in a setting that is conducive to open discussion.
A Wide Variety of Support Services
In Germany, the Psychotrauma Centre of the Bundeswehr Hospital Berlin offers workshops for couples, workshops for family members and family retreats for the Bundeswehr in cooperation with the Office of the Protestant Church for the Bundeswehr (EKA). The EKA also runs the ASEM project (“Field of Activity: Pastoral Care for Persons Suffering from Deployment-Related Disorders”). This project is supported by various institutions closely cooperating with the Bundeswehr and by the Bundeswehr itself. It provides Bundeswehr personnel who have lost someone close to them or who have experienced physical and/or mental stress with an opportunity to share their experience and recuperate. The Protestant Association for Care and Welfare of Military Personnel (EAS) and the Catholic Association for Care and Welfare of Military Personnel (KAS) also organise recreational activities for families and couples and holiday camps for children.
Other institutions closely cooperating with the Bundeswehr also offer support to family members, such as the “Support Network” for military personnel, reservists, veterans and families, which comprises various organisations. Its target group includes surviving family members, persons who have sustained physical or mental injuries, military personnel suffering from deployment-related stress and their families, former military personnel and their families, active Bundeswehr personnel, persons providing psychosocial support for affected individuals and their families, and members of non-military organisations. The Bundeswehr Social Services provide advice and support on all social matters for Bundeswehr personnel and their families. They also focus on former Bundeswehr personnel and surviving family members.
This list of support services is not exhaustive but is meant to provide an idea of the existing services that are available in addition to post-deployment seminars, which have also been opened up to families of military personnel.
“Relationships and PTSD” Workshop for Family Members
Since 2011, the Psychotrauma Centre of the Bundeswehr Hospital Berlin has offered and run psychoeducative workshops for family members in cooperation with the EKA. Titled “Relationships and PTSD – A Workshop for Family Members”, these weekend workshops provide couples with the opportunity to come to terms with the PTSD diagnosis. These workshops are intended for traumatised military personnel and their partners. They focus on viewing couples as couples and not as parents. Their aim is to provide psychoeducation regarding PTSD or other post-traumatic disorders and to establish a network for family members. The workshops are conducted by Bundeswehr social workers, a physician specialising in psychotherapy and a military chaplain. These therapists are able to work very closely with the patients and their partners, as a maximum of five couples participate in each workshop.
Workshops for family members are comprised of three modules. The first module is prepared separately by family members and patients and is primarily about providing information; the second module focuses on emotional relief and the third deals with the strengthening of resources. The aim of the workshops is to strengthen the couples’ relationships.
A study on the effectiveness of the workshops confirmed that there was a significant increase in physical, mental and overall quality of life of family members. There was also a much greater sense of reciprocity such that the support provided by each partner was more well-balanced. These results may be seen as indications that workshops for family members are having a positive effect on the quality of life of family members of military personnel suffering from PTSD [26].
Purpose
This study deals with problem areas described by family members of military personnel suffering from PTSD. It focuses on deployment-related changes. The article seeks to answer the following questions:
- Can the problem areas of affected persons described by family members be categorised?
- If problem areas are mentioned, do they have any effects on the relationship?
- Do any of the problem areas match the diagnostic criteria for PTSD according to the ICD-10?
Methodology
“Do you feel that something has changed as a result of your partner's deployment-related problems? YES/NO.
If the answer is YES, please give examples.”
Respondents were free to choose which examples they provided. In this context, the term “family members” refers exclusively to the partners of military personnel.
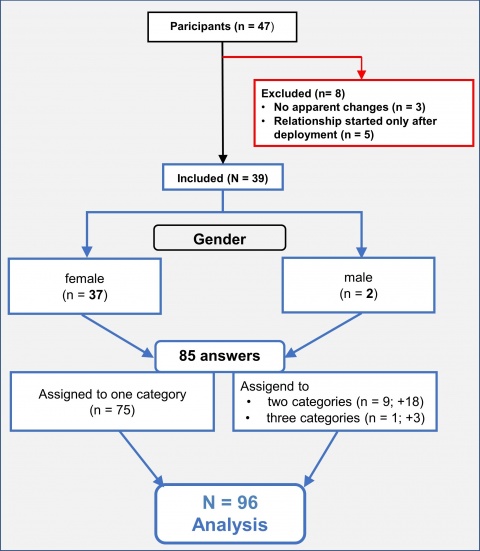
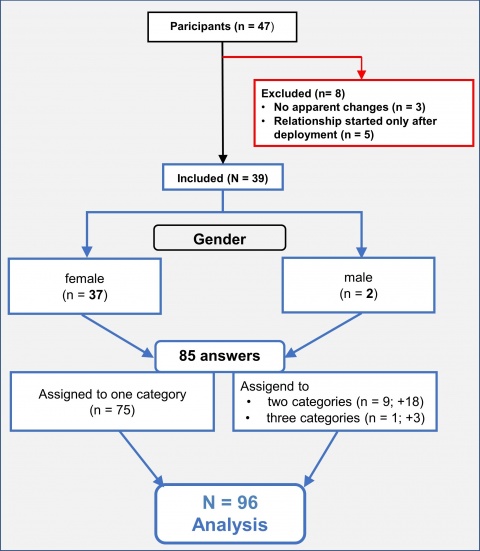
Three out of the 47 family members who participated in the workshop were excluded from this study because they stated that they did not notice any apparent changes. Another five persons were excluded because in each case their relationship had only started after deployment abroad and they were thus unable to provide information with regard to any changes. This left 39 data sets to be analysed. These 39 data sets include 37 from female family members and 2 from male family members. A gender-specific analysis was therefore unnecessary. A detailed list can be found in the flow diagram in Figure 1. The family members’ ages ranged from 21 to 60 years, with an average age of 33.9 years (median: 34 years). 56% of participants said that they had children.
The data sets were evaluated according to the six phases of thematic analysis developed by BRAUN and CLARKE [3]. A theme is defined as important in relation to the amount of data available and the purpose of the study. The relevant themes are developed as categories derived from the answers. These answers are then assigned to the categories. After that, a cumulative evaluation of the answers in the individual categories is performed, with the option to assign an answer to multiple categories. Finally, the categories are ranked according to absolute cumulative frequency. When using this methodological approach, it must be assumed that family members primarily mention those problem areas which seem most important or urgent to them. A detailed description of the phases can be found in BRAUN and CLARKE’s method description [3].
Two independent evaluators (“raters”) developed the categories and assigned the questions. One category (changes in personality and behaviour) was included only after consultation between the two raters. One rater’s assignment of items to a category matched the other rater’s assignment in 95.8% of cases. Final assignment of items to a category was achieved by consensus between the raters.
Results
The answer to the first part of the question whether the partners of military personnel felt that anything had changed as a result of the deployment-related problems was “Yes” for 83% of the participants (39 out of 47), “No” for 6.4% (3 out of 47), and 10.6% did not provide any answer (5 out of 47). Based on item analysis, 9 categories were developed. Regarding the second part of the question, “If the answer is yes, please give examples”, 39 respondents provided a total of 85 examples. Nine items were assigned twice and one item was assigned three times, so that a total of 96 statements were assigned to nine categories (see Figure 1). This corresponds to an average of 10.6 answers per category. The following categories have been ranked in descending order according to absolute cumulative frequency. Sample answers can be found in Table 1.
Feelings and Emotions Expressed
Most statements, amounting to 17.7% of all items, belonged to the category of feelings and emotions expressed. Frequently mentioned items included anxiety, depression, pessimism, a bad mood or callousness. In addition to the anxiety that family members observe in their military partners, the main element in this category is the service member’s failure to express their feelings. Mood swings, irritability and a short temper were also mentioned.
Withdrawal and Avoidance Behaviour
Withdrawal and/or avoidance behaviour exhibited by their military partners made up 15.6% of family members’ statements. The examples given by respondents can be further divided into behaviour exhibited in public and private spaces and into avoidance behaviour at the interpersonal level. Crowds, public transport, public events and driving were cited as areas or activities that were avoided. In the private sphere, family members described their partners withdrawing from family gatherings and from family life in general. Family members also observed that, in addition to the above-mentioned behaviour, their military partners were guarded, detached and reclusive. This also affects the interpersonal level in their relationships. A lack of interest, avoiding closeness and keeping secrets were mentioned as examples.
Aggression and Hostility
14.6% of statements were assigned to this category. Hostility was expressed as a high degree of aggressiveness when loved ones were threatened. Aggression was also evident in verbal communication, increased irritability and testiness, as well as a quick and impulsive temper.
Communication
Communication was the fourth-largest category with 11.5% of responses. The focus in this category was on a decrease in communication and conversation. These changes were evident from service members having fewer conversations, keeping secrets and lying. Another major element in this category was verbally aggressive behaviour. Conflicts were caused by intermittent communication difficulties. Another problem for family members was the feeling of having to be extremely careful about what they said to their partners. This was the case especially when both partners were in the military.
Physical Closeness
10.4% of statements concerned physical closeness between partners, which had changed as a consequence of deployment-related PTSD. This category’s focus is on the couples’ sex lives. According to half of the statements made in this category, couples experienced difficulties in their sex lives and sometimes had no sex lives at all. In addition, the family members described having experienced situational changes regarding physical closeness or complete physical distance from their partners.
Trust
Other statements (9.3%) described the problem area of trust. This refers to being dishonest and taciturn within the relationship and, at the same time, to a feeling of insecurity because of the physical environment. Participants mentioned their partners “scanning their surroundings” as one of the signs showing their distrust of the environment.
Physical Symptoms
Another 9.3% of statements referred to physical symptoms. In this category, the focus is on sleep disorders including nightmares, poor quality of sleep, difficulties falling or staying asleep and sleeplessness. Other symptoms included lack of concentration, quick exhaustion or restlessness.
Residual Category
6.3% of the statements could not be assigned to any other problem area and thus form their own independent residual category. Due to the open nature of the question, participants gave very different answers. This category was therefore not further evaluated.
Changes in Personality and Behaviour
5.2% of the statements referred to a dramatic change in the personality of military personnel suffering from PTSD. One of the aspects mentioned was the disappearance of an essential character trait such as humanity or the person’s entire identity.
Table 1: Category ranking with example items
Rank | Category | Examples |
1 | Feelings and Emotions Expressed | “he doesn’t show his feelings any more”, “he is afraid”, “I have become worthless” |
2 | Withdrawal and Avoidance Behaviour | “introspective”, “solitary”, “avoidance of large crowds” |
3 | Aggression and Hostility | “partner’s mood changes by the minute”, “irritable, more impatient”, “partner is emotionally cold” |
4 | Communication | “verbally aggressive”, “more arguments”, “trust has become difficult”, “poor communication”, “often offended” |
5 | Physical Closeness | “physical distance”, “no sex life”, “does not tolerate closeness” |
6 | Trust | “scanning the surroundings”, “no openness”, “relationship to each other” |
7 | Physical Symptoms | “many nightmares”, “less resistance to stress”, “restlessness”, “often lacks concentration” |
8 | Residual Category | “roles have changed”, “restrictions in everyday life and in the family” |
9 | Changes in Personality and Behaviour | “just no longer the man I came to know and love”, “has lost his humanity” |
Discussion
Since a complete survey was conducted, data quality is very good. The examples mentioned by family members were easily categorised. There was an average of 10.6 statements per category. Out of a total of 96 statements, 93.8% could be attributed to one of the eight identified problem areas.
All identified categories directly or indirectly affect the relationship. As illustrated in the category “feelings and emotions expressed”, the affected servicemen and women are no longer able to adequately express their affections and emotions. More reserved behaviour and a withdrawal from everyday life, being part of the category “withdrawal and avoidance behaviour”, also have a mostly negative impact on the relationship. Tasks and roles must often be rearranged. Avoidance symptoms are often directly related to dysfunctional family relationships [10]. Partners sometimes even support and reinforce avoidance behaviour out of consideration for the affected serviceman or woman.
The effect of “aggression and hostility” on relationships is obvious. GALOVSKI and LYONS [10] identified a connection between the anger veterans suffering from PTSD feel and dysfunctional family relationships, as well as secondary traumatisation of other family members. Previous studies conducted within the Bundeswehr found that aggression and hostility were early behavioural indicators of a later development of post-traumatic stress symptoms [12, 32]. They also found that policemen and women, in comparison with other emergency services personnel, showed increased hostility after the terrorist attack on the Christmas market in Berlin. This is attributed to the various functions and tasks during operations [31]. Verbal aggression also has an undesirable effect in the problem area “communication”. Changes in the area “physical closeness” often relate to sexuality. MANSO, TAFT and FREDMAN [16] consider PTSD in service personnel to be a cause of problems in intimate relationships. A lack of trust in the relationship, but also in the person’s surroundings, also affects the relationship.
“Physical symptoms” such as restlessness and sleep disorders affect the sleep quality of persons with PTSD. In most cases, they share a bed with their partners who thus have first-hand experience of the affected person’s sleep disorders and of the person’s sleep being interrupted by nightmares. Studies regarding sleep and nightmares in Bundeswehr military personnel suffering from deployment-related stress also prove this [6- 8]. Certain character and personality traits make people fall in love with each other. If a personality change occurs that causes a dramatic change in the partner’s character, this will affect the relationship. In extreme cases, it may even lead to separation. The divorce rate of World War II veterans suffering from PTSD, for example, is higher than that of unaffected World War II veterans [5].
Diagnostic Criteria according to the ICD-10
Some aspects of the selected categories match the diagnostic criteria for post-traumatic stress disorder (F43.1) according to the ICD-10 (see Table 2).
Table 2: Diagnostic Criteria for Post-Traumatic Stress Disorder according to the ICD-10
Diagnostic Criteria for PTSD according to the ICD-10 | |
A | Exposure to an event or situation (either brief or long-lasting) of an exceptionally threatening or catastrophic nature, which is likely to cause pervasive distress in almost anyone. |
B | Constantly remembering or reliving the trauma in intrusive memories (“flashbacks”), vivid memories, recurring dreams, or distress when exposed to situations reminiscent of the trauma. |
C | Actual or preferred avoidance of situations that remind the sufferer of the original trauma. This behaviour was not present before the traumatic experience. |
D | Either of the following is present:
|
E | Criteria B, C and D usually arise within 6 months of the traumatic event or at the end of a period of stress. (In some special cases, onset delayed more than 6 months can be included, but this should be clearly specified). |
The category “aggression and hostility” corresponds roughly to criterion D.2.b. of the ICD-10, “irritability or outbursts of anger”. The category “withdrawal and avoidance behaviour”, too, is reflected in criterion C of the ICD-10: “Actual or preferred avoidance of situations that remind the sufferer of the original trauma. This behaviour was not present before the traumatic experience.”
In addition to the avoidance of certain situations, partners also described withdrawal behaviour and avoidance at the interpersonal level, which are not explicitly included in the ICD-10 as diagnostic criteria. The physical symptoms mentioned by partners are included in the ICD-10 in criterion D.2.a (“difficulty in falling or staying asleep”) and D.2.c (“difficulty concentrating”).
“Feelings and emotions expressed” must be considered a mixed category. Some of the problems mentioned can be assigned to criterion B (“constantly remembering or reliving”), but the majority of them concern the current mood of the affected persons or the feelings they show to their partners.
The changed personality of affected persons is not directly listed in the diagnostic criteria. The present study will not go into detail on the diagnosis of “enduring personality change after catastrophic experience” (F62.0) in our study.
The remaining categories are not part of the ICD-10. Physical closeness is not a diagnostic criterion but an important element of a relationship. At another level, it can be a factor that allows a partner “early recognition” of an illness.
Outlook
The deployment-related psychological changes in affected service personnel described by their family members are predominantly serious symptoms of clinical relevance. We were able to prove their direct and indirect effects on family members. The identified categories allow us to develop more specific measures that focus on family members. There are at present considerations to develop new group therapies that take these findings into account. Due to limited resources, however, the feasibility of such therapies must still be examined.
The identified categories are also intended to help develop a questionnaire for family members to help increase their awareness of their partners’ problems. If there are any noticeable signs, they can talk to their partners about the problem at an early stage. Involving families may potentially shorten the latency period between the onset of symptoms and the initiation of treatment and also increase the use of support services. Since the overwhelming majority of service personnel suffering from mental problems never seek professional help [35], this could help to deal with one of the most significant challenges currently facing military psychologists, psychiatrists and social workers. To our knowledge, there has so far been no approach in this regard. Should our approach prove successful, it could also be adopted for emergency services personnel such as police or firefighters.
Literature
- Back D, Walsmann K, Hauer T, Huschitt N, Bowyer MW, Wesemann U, Lieber A, Willi C: Concept and evaluation of the German War Surgery Course – Einsatzchirurgie-Kurs der Bundeswehr. J R Army Med Corps 2017; 163(3): 206-210.
- Bandelow B, Koch M, Zimmermann P, Biesold KH, Wedekind D, Falkai P: Posttraumatic stress disorder (PTSD) in the German Armed Forces: A retrospective study in inpatients of a German army hospital. Eur Arch Psychiatry Clin Neurosci 2012; 262(6): 459-467.
- Braun V, Clarke V: Using thematic analysis in psychology. Qualitative Research in Psychology 2006; 3(2): 77-101.
- Butler O, Herr K, Willmund G, Gallinat J, Zimmermann P, Kühn S: Neural correlates of response bias: Larger hippocampal volume correlates with symptom aggravation in combat-related posttraumatic stress disorder. Psychiatry Res Neuroimaging. 2018; 279: 1-7.
- Cook JM, Riggs DS, Thompson R, Coyne JC, Sheikh JI: Posttraumatic stress disorder and current relationship functioning among World War II ex-prisoners of war. In: Journal of family psychology JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2004; 18(1): 36-45.
- Danker-Hopfe H, Sauter C, Kowalski JT, et al.: Sleep quality of German soldiers before, during and after deployment in Afghanistan – a prospective study. JSleepRes 2017; 26(3): 353-363.
- Danker-Hopfe J, Sauter C, Kowalski JT, Kropp S, Ströhle A, Wesemann U, Zimmermann P: Effect of deployment related experiences on sleep quality of German Soldiers after return from an International Security Assistance Force (ISAF) mission to Afghanistan. Psychiatry Research 2018; 270: 560-567.
- de Dassel T, Wittmann L, Protic S, Höllmer H, Gorzka RJ: Association of posttraumatic nightmares and psychopathology in a military sample. Psychol Trauma. 2018; 10(4): 475-481.
- Gabriel U, Jacobsen T, Hauffa R, Zimmermann P, Kowalski J: Evaluation des telefonischen Beratungsangebotes für Soldaten mit einsatzbedingten psychischen Belastungen und deren Angehörige. Wehrmedizinische Monatsschrift 2011; 55(10):228-230.
- Galovski T, Lyons, JA: Psychological sequelae of combat violence. A review of the impact of PTSD on the veteran’s family and possible interventions. In: Aggression and Violent Behavior 2004: 9(5): 477-501.
- Himmerich H, Willmund GD, Zimmermann P, Wolf JE, Bühler A, Holdt LM, Teupser D, Kirkby KC, Wesemann U: Serum concentrations of soluble TNF receptor p55 (sTNF-R p55) correlate with post-traumatic stress symptoms in German soldiers after deployment abroad. Eur Cytokine Netw 2015; 26(3): 57-60.
- Himmerich, H, Wesemann U, Dalton B, Holdt LM, Teupser D, Willmund GD: Exploring an association between hostility and serum concentration of TNF-α and its soluble receptors. J Psychosom Res2016; 91: 87-88.
- Höllmer H: Traumafolgestörungen im militärischen Kontext. Nervenheilkunde 2016; 35: 465-468.
- Kasselmann N, Bickelmayer J, Peters H, Wesemann U, Oestmann JW, Willy C, Back DA: Relevanz der Einsatz- und Katastrophenmedizin für Medizinstudierende: Eine Pilotevaluation im Rahmen einer interdisziplinären Vorlesungsreihe. Der Unfallchirurg 2019; in print.
- Kuester A, Köhler K, Ehring T, et al.: Comparison of DSM-5 and proposed ICD-11 criteria for PTSD with DSM-IV and ICD-10: Changes in PTSD prevalence in military personnel. Eur J Psychotraumatol. 2017; 8:1, DOI; 10.1080/20008198.2017.1386988.).
- Manson CM, Taft TC, Fredman JS: Military-related PTSD and intimate relationships. From description to theory-driven research and intervention development. In: Clinical psychology review 2009; 29(8): 707-714.
- Muschalla B, Rau H, Willmund G, Knaevelsrud C: Work disability in soldiers with posttraumatic stress disorder, posttraumatic embitterment disorder and not-event-related common mental disorders. Psychological Trauma Theory Research Practice and Policy 2018; 10(1):30-35.
- Rose C, Zimmermann P: Belastungen von Angehörigen im Kontext psychischer Traumatisierungen. J Deradicalization 2015; 15(2): 1-20.
- Rose C: Angehörigenarbeit. In: Peter L. Zimmermann und Volker Eisenlohr (Hrsg.): Psychosoziale Belastungen. Eine Orientierungshilfe für Mitglieder des Psychosozialen Netzwerkes der Bundeswehr. 2. Aufl. Berlin: Psychotraumazentrum am Bundeswehrkrankenhaus 2015; 29-32.
- Rüsch N, Rose C, Holzhausen F, Mulfinger N, Krumm S, Corrigan PW, Willmund GD, Zimmermann P: Attitudes towards disclosing a mental illness among German soldiers and their comrades. Psychiatry Res 2017; 258: 200-206.
- Schura R, Wesemann U, Zimmermann P, Kropp S: Zigarettenabhängigkeit bei Soldaten der Bundeswehr. Wehrmedizinische Monatsschrift 2015; 59(2): 38-41.
- Siegl S, Rau H, Dors S, et al.: Barriers to treatment-seeking among German veterans: Expert interviews. ZEFQ 2017; 125: 30-37.
- Trautmann S, Schönfeld S, Behrendt S: Substance use and substance use disorders in recently deployed and never deployed soldiers. Drug Alcohol Depend. 2014; 134: 128-135.
- Ungerer, J.; Zimmermann, P. (2015): Psychotraumatologie. In: Christan Neitzel und Karsten Ladehof (Hg.): Taktische Medizin, Notfallmedizin und Einsatzmedizin. 2. Aufl. 2015. Berlin: Springer Berlin: 335-344.
- Wesemann U, Jensen S, Kowalski JT, et al.: Einsatzbedingte posttraumatische Belastungsstörung im sozialen Umfeld von SoldatInnen – eine explorative Studie zur Entwicklung und Evaluierung eines Angehörigenseminars; Trauma und Gewalt 2015; 9 (3): 216-225.
- Wesemann U, Kowalski JT, Jacobsen T, Beudt S, Jacobs H, Fehr J, Büchler J, Zimmermann PL: Evaluation of a technology-based adaptive learning and prevention program for stress response – a randomized controlled trial. Mil Med 2016; 181(8): 863-871.
- Wesemann U, Kowalski JT, Zimmermann P, Rau H, Muschner P, Lorenz S, Köhler K, Willmund GD: Vom Helden zum Profi – Veränderung der Einstellung zu psychischen Erkrankungen bei Einsatzsoldaten durch das präventive Computerprogramm CHARLY Wehrmedizinische Monatsschrift 2016; 60(1): 2-7.
- Wesemann U, Mahnke M, Polk S, Bühler A, Willmund G: Impact of crisis intervention on the mental health status of emergency responders following the Berlin terrorist attack in 2016. Disaster Med Public Health Prep 2019; in print.
- Wesemann U, Schura R, Kowalski JT, Kropp S, Danker-Hopfe H, Rau H, Ströhle A, Thiele J, Zimmermann PL: Context of deployment and tobacco dependence among soldiers; Gesundheitswesen 2015; 511: 1-6.
- Wesemann U, Willmund GD, Ungerer D, et al.: Assessing Psychological Fitness in the Military Development of an Effective and Economic Screening Instrument. Mil Med 2018; 183(7-8): e261-e269.
- Wesemann U, Zimmermann P, Mahnke M, Butler O, Polk S, Willmund G: Burdens on emergency responders after a terrorist attack in Berlin. Occup Med (Lond). 2018; 68(1): 60-63.
- Wesemann U, Zimmermann PL, Bühler A, Willmund GD: Gender Differences in Hostility and Aggression Among Military Healthcare Personnel After Deployment. J Womens Health (Larchmt). 2017; 26(10): 1138.
- Willmund G, Alliger-Horn C, Kowalski JT, Zimmermann P: Dolphin-Assisted Therapy in the Treatment of Bundeswehr Soldiers with Deployment-Related Post-Traumatic Stress Disorder. European Journal of Integrative Medicine 2013 (Published on reasearchgate.net).
- Willmund G, Heß J, Helms C, et al.: Suicides between 2010 and 2014 in the German Armed Forces – Comparison of Suicide Registry Data and a German Armed Forces Survey. Suicide Life Threat Behav 2019; in print.
- Wittchen HU, Schönfeld S, Kirschbaum C, et al.: Traumatic experiences and posttraumatic stress disorder in soldiers following deployment abroad: How big is the hidden problem? Dtsch Ärztebl Int. 2012; 109(35-36): 559-568.
- Zimmermann P, Alliger-Horn C, Köhler K, et al.: Depressivität und Wertorientierungen im Verlauf von militärischen Auslandseinsätzen. Trauma und Gewalt 2018; 12(2): 134-150.
- Zimmermann P, Kahn C, Alliger-Horn C, et al.: Assoziation von Werteorientierungen mit der Schwere einer Alkoholabhängigkeit bei Soldaten in qualifizierter Entzugsbehandlung. Nervenheilkunde 2015; 10: 803-808.
Citation
Wesemann U, Radszat S, Fischer T, Rose C: Perception of family members and relatives on military personnel with deployment-related posttraumatic stress disorders – a qualitative evaluation of an activatable resource. Wehrmedizinische Monatsschrift 2019; 63(3-4): 73-79.
For the authors
Dr. Ulrich Wesemann, Chief Psychologist
Psychotrauma Centre of the Bundesweh
Bundeswehr Hospital Berlin
Scharnhorststr. 13, 10115 Berlin
E-Mail: [email protected]
Datum: 24.04.2019