
Interdisciplinary Treatment of Spinal Injuries and Bone Metastases Using 3D Robotic Fluoroscopy
Department of Radiology¹ (Head of Department: Dr S. Waldeck, Colonel (MC)) and Department of Trauma Surgery and Orthopaedics² (Head of Department: Dr E. Kollig, Assistant Professor and Colonel (MC)) of the Bundeswehr Central Hospital in Koblenz (Hospital Commander and Medical Director: A. Nolte, Brigadier (MC))
Kai Nestler¹, Benjamin V. Becker¹, Daniel A. Veit¹, Erwin Kollig², Stephan Waldeck¹
Abstract
The rapid progress of radiological technology and robotics opens up new opportunities for the interdisciplinary treatment of surgical and internal medicine conditions that thus far have been managed by a single area of specialisation.
Two case studies of vertebral body injuries in patients treated at the Bundeswehr Central Hospital in Koblenz are used to demonstrate the opportunities presented by the interdisciplinary use of robot-assisted radiological systems. The authors also discuss how this technology could be used to treat mission-related injuries.
Keywords Percutaneous vertebroplasty, kyphoplasty, needle guidance, Dyna CT, radiofrequency-targeted vertebral augmentation
Introduction
The rapid progress in radiological technology opens up new opportunities for the interdisciplinary treatment of conditions that were previously managed by a single area of medical specialisation. A good example of this approach is the treatment of spinal conditions such as traumatic fractures and potential vertebral fractures caused by metastatic disease. Such conditions are now being managed by robot-assisted angiography at the Bundeswehr Central Hospital in Koblenz.
Problem
There is a high incidence of traumatic spinal injuries caused by high-energy blunt or penetrating impact [6]. Such injuries are seen in deployed settings following attacks on armoured vehicles [5]. Spinal metastatic disease occurs in 60-70% of patients with systemic cancer [7] and is thus also found in soldiers.Interdisciplinary minimally invasive therapy, e.g. kyphoplasty or spinal fusion using fluoroscopic x-ray guidance, is increasingly being employed by physicians [2]. This is a result of the progress made in this therapeutic approach and the effectiveness of this low-risk treatment and is reflected in the increased number of operations.
Robot-assisted fluoroscopy expands previous treatment options and makes surgery more accurate with fewer complications. It does not involve the restrictions of intraoperative fluoroscopy using a conventional C-arm [8] (Figure 1).
Procedure
Percutaneous vertebroplasty is a minimally invasive operation which uses fluoroscopic x-ray guidance to inject bone cement to stabilise vertebral bodies. With the patient in a prone position, a needle is advanced through the pedicle and into the vertebral body by radiologists and trauma surgeons/orthopaedists working in an interdisciplinary team. A robot-assisted flat panel detector angiography system makes possible peri-interventional 3D imaging, what is known as Dyna computed tomography (Dyna CT). Access can thus be planned in all dimensions and monitored during surgery. In addition to exactly showing the access route by CT, this system uses a laser to project the correct angulation at skin level (Figure 2). This allows the vertebral body to be punctured safely and exactly.A probe is then used to prepare the vertebral body. The cavities created are filled by way of radiofrequency-targeted vertebral augmentation [4]. In this procedure, radiofrequency is used to activate high-viscosity cement that then hardens. Combined with exact position control, this procedure reduces risks such as extraosseous cement leakage [9].
This highly precise intervention also enables the targeted management of osseous metastases in order to prevent and treat pathological fractures in the spinal and pelvic areas. An interdisciplinary tumour board decides on the treatment, which is then conducted on a multidisciplinary basis. In this context, radiofrequency ablation increases the treatment options available, as a robot can assist with the exact placement of the probe.
Case Reports
We present the cases of two patients who received interdisciplinary treatment with minimally invasive technology and robot-assisted fluoroscopy. One patient had a traumatic vertebral body injury, the other one had painful osseous metastases that threatened the stability of the spine. Neither patient experienced complications. Peri-interventional Dyna CT made it possible to assess the outcome of treatment even before the intervention was completed.
Case 1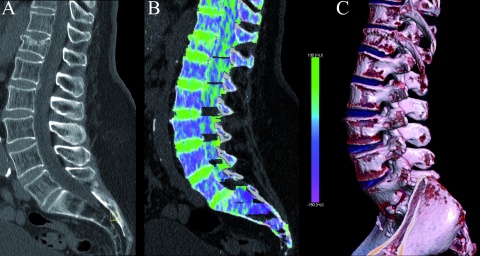
Soldier, aged 37, after a fall
Figure 3A shows an endplate trauma fracture of the anterior edge. A dual energy CT was used to visualise the new vertebral oedema (Figure 3B). A 3D reconstruction (Figure 3C) shows a wedge-shaped vertebral body with a wide base.

A 3D rotational data set was generated for a final assessment and showed that the vertebral body was sufficiently filled, the endplate was successfully raised, and the position of intravertebral cement was suitable (Figure 4C).
Case 2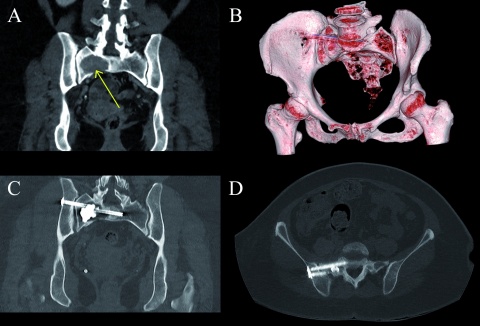
Female patient, aged 58, with osteolytic bone metastases from non-small-cell lung cancer
Figure 5A shows painful osseous metastases on the right side of the sacrum which may have compromised spinal stability. The tumour board decided on multidisciplinary treatment.
To treat the lytic lesion, a probe was first placed using robot-assisted radiofrequency ablation. Radiofrequency-targeted vertebral augmentation was performed via a lateral access route to stabilise the affected area (Figure 5C). The pelvis was stabilised immediately afterwards by screw fixation of the sacroiliac joint via the lateral iliac bone (Figures 5B–D). Stabilisation and a substantial reduction in pain were achieved by the combined therapy.
Way ahead
The treatment of complex conditions demands increased interdisciplinary cooperation, particularly on account of the rapid technical progress made in robot-assisted fluoroscopic systems. The cases presented here show that low-risk operations with good outcomes are possible. Complications, particularly nerve and vascular injuries, and the risk of cement leakage are reduced [1]. The interdisciplinary approach also broadens the range of treatment options and opens up additional opportunities for using osteosynthesis [3]. Especially peri-interventional assessments by means of Dyna CT can lead to new uses in future.
Auxiliary systems such as needle guidance allow surgeons with less practical experience to perform safe surgery. In addition to their timely use in Bundeswehr hospitals after aeromedical evacuation, such systems could also be used in the future to expand treatment options in deployed settings.
Literature
- Baroud G, Crookshank M, Bohner M: High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine 2006; 31(22): 2562-2568.
- Coronel EE, Lien RJ, Ortiz AO: Postoperative spine imaging in cancer patients. Neuroimaging Clinics 2014; 24(2): 327-335.
- Doerfler A, Gölitz P, Engelhorn T, Kloska S, Struffert T: Flat-panel computed tomography (DYNA-CT) in neuroradiology. from high-resolution imaging of implants to one-stop-shopping for acute stroke. Clinical neuroradiology 2015; 25(2): 291-297.
- Petersen A, Hartwig E, Koch EMW, Wollny M: Clinical comparison of postoperative results of balloon kyphoplasty (BKP) versus radiofrequency-targeted vertebral augmentation (RF-TVA): a prospective clinical study. European Journal of Orthopaedic Surgery & Traumatology 2016; 26(1): 67-75.
- Ragel BT, Allred CD, Brevard S, Davis RT, Frank EH: Fractures of the thoracolumbar spine sustained by soldiers in vehicles attacked by improvised explosive devices. Spine 2016; 34(22): 2400-2405.
- Schoenfeld AJ, Newcomb RL, Pallis MP et al.: Characterization of spinal injuries sustained by American service members killed in Iraq and Afghanistan: a study of 2,089 instances of spine trauma. Journal of trauma and acute care surgery 2013; 74(4): 1112-1118.
- Shah LM, Salzman KL: Imaging of spinal metastatic disease. International journal of surgical oncology 2011; Article ID 769753
- Wallace MJ, Kuo MD, Glaiberman C, Binkert CA, Orth RC, Soulez G, Technology Assessment Committee of the Society of Interventional Radiology: Three-dimensional C-arm cone-beam CT: applications in the interventional suite. Journal of Vascular and Interventional Radiology 2008; 19(6): 799-813.
- Yang PL, He XJ, Li HP; Zang QJ, Wang GY: Image-guided minimally invasive percutaneous treatment of spinal metastasis. Experimental and therapeutic medicine 2017; 13(2): 705-709.
- Zhan Y, Jiang J, Liao H, Tan H, Yang K: Risk factors for cement leakage after vertebroplasty or kyphoplasty: a meta-analysis of published evidence. World neurosurgery 2017; 101: 633-642.
Images: Department of Radiology, Bundeswehr Central Hospital, Koblenz
Citation
Nestler K, Becker BV, Veit DA, Kollig E, Waldeck S: Interdisciplinary Treatment of Spinal Injuries and Bone Metastases Using 3D Robotic Fluoroscopy Wehrmedizinische Monatsschrift 2019; 63(2): 86-88.
For the authors
Dr. Kai Nestler, Squadron Leader (MC)
Bundeswehr Central Hospital, Koblenz
Department of Radiology
Rübenacher Str. 170, 56072 Koblenz
Email: kai1nestler@bundeswehr.org
Datum: 26.04.2019











